PHOENIX — As more patients are admitted for COVID-19, hospitals across the state are trying to make more room.
Banner Health said Friday that several of their local hospitals have activated surge plans while others are getting closer to capacity.
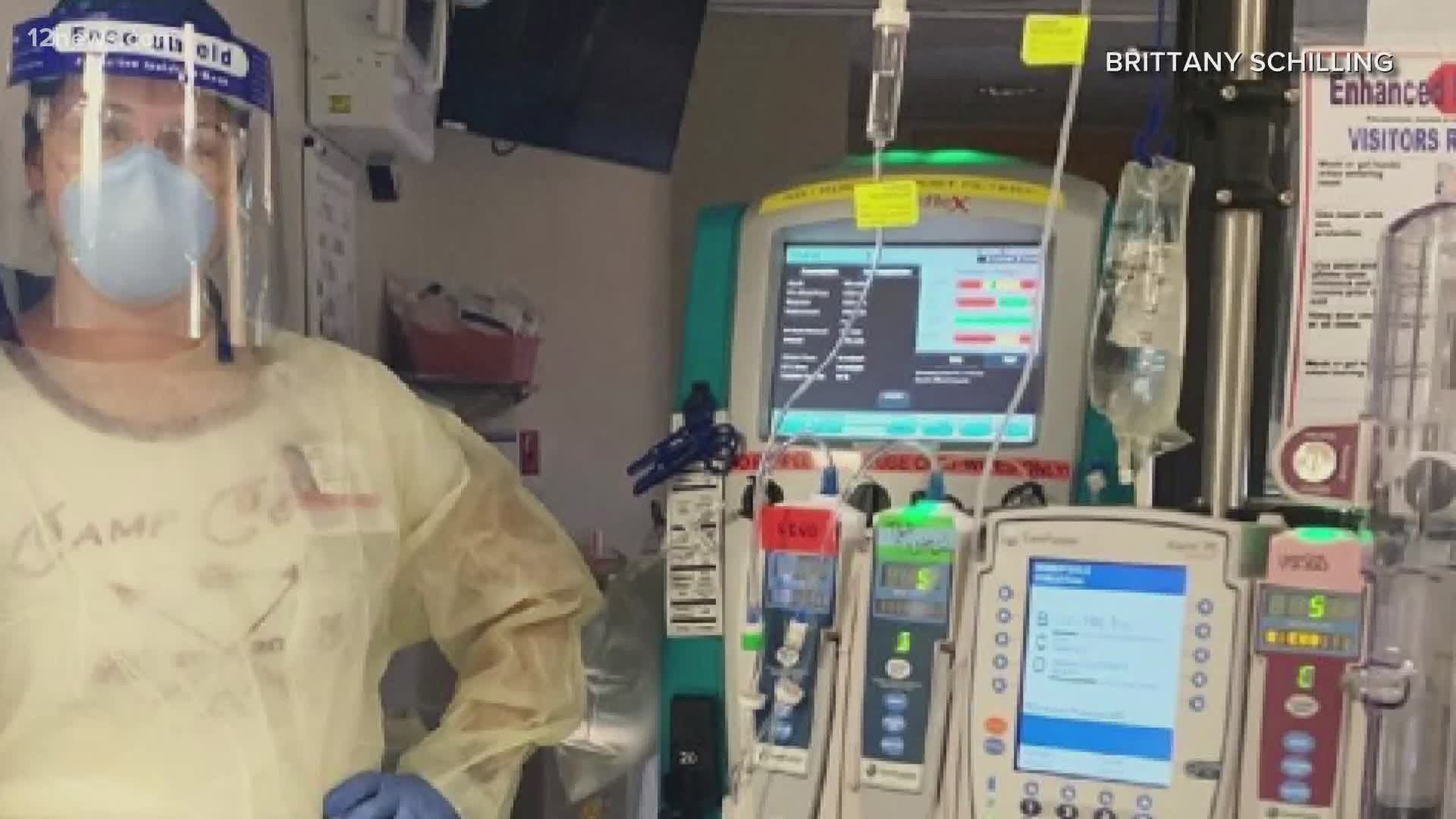
"The second you walk in those doors, you just don’t know what’s coming," said Brittany Schilling.
Schilling is an ICU nurse at Banner UMC in Phoenix, where she’s seen a range of COVID-19 patients. She says she's seen people of all ages being admitted, but since Memorial Day, many of her patients have been in the 20-45 range.
"The scary thing about this disease and the heartbreaking thing is they can turn so quickly," she said. "They are texting in their bed and we look at their chest X-Rays and say, 'This is not good.' And within a few hours, they’re on the ventilator and on life-sustaining medication. It just happens very quickly."
She says three of their six ICUs are for COVID patients and space isn’t always as it seems.
"Yes, we do have 'capacity' available, but that looks like using these beds we normally wouldn’t use and having patients in conference rooms," Schilling said.
Dignity Health says they've set up air-conditioned tents outside of St. Joseph's Hospital and Chandler Regional Medical Center to help make more room. The tents would be used to care for non-COVID patients with less urgent needs.
"We are really in a tough spot and every day we go to work is worse than the one before it," Schilling said.
As more patients come in, she says there’s a need for more nurses.
"The hardest part is just using our time wisely with these ICU patients," Schilling explained. "Giving them the care that they need, but also facing the need to take on more patients per nurse because we just don’t have the staffing right now.
Banner Health says they're working to increase staff as the number of patients rise. That includes contracting nurses from out of state and also bringing other healthcare workers out of retirement.
It’s the same problem Phoenix nurse Rayna Sloane saw weeks ago when she went to the Washington D.C. area to help care for COVID-19 patients.
"Your normal ratio for ICU nurses is one nurse to two patients," Sloane said. "They’re just overwhelmed, you’re taking three patients, you’re everywhere."
The job is non-stop: checking vitals, checking medicines, sometimes watching patients take their last breath.
"It’s always hard losing a patient," Schilling said. "The hardest part is family not being able to be there to say goodbye. I’ve had many heart-wrenching and very tearful discussions over FaceTime with the family as they say goodbye to their loved one."
Sloane echoes the heartbreak that comes with losing a patient. And she says it becomes more difficult when that nurse to patient ratio keeps increasing.
"It’s a fear," she said. "Am I being a good enough nurse?"
Sloane is back in Arizona now, getting ready to start a new job as a nurse practitioner at another hospital.
She had hoped what she saw on the East Coast wouldn’t haunt hospitals here.
"I don't know what I'll be walking into," she says.
Both nurses are also begging the public to wear masks and wash their hands. They’ve seen with their own eyes how COVID-19 can affect all age and they don’t want to see you next in their hospital.