PHOENIX — When Tony Robles’ father Antonio tested positive for COVID-19, the rest of the family let their guard down.
Antonio was a healthy man. He drank green juice. Walked several miles through the neighborhood every day. Had no pre-existing health conditions and was only 56 years old.
Even after Antonio was hospitalized, his health care providers thought he would recover. He was strong, and despite the challenges in the hospital, after the first week he was there, he seemed to be getting better.
But Tony began to worry when his father had an accident in the hospital; his nurses and other hospital staff were unable to respond to help Antonio make it to the restroom in time, and Antonio soiled himself.
That’s when Tony Robles began recording phone calls with hospital staff – asking what he could do to try and save his father’s life.
Crisis In Care
On Jan. 26, 2020, the Arizona Department of Health Services confirmed the first person in Arizona had tested positive for COVID-19.
One year later, Arizona has experienced shutdowns, curfews, limitations on our abilities to see loved ones in the hospital or nursing homes – all to protect the states’ most vulnerable and protect hospitals from overcrowding.
Still, some health care providers and researchers argue what mitigation measures that have remained in place are not enough to combat the pandemic.
And on July 8, 2020 -- the day Antonio Robles was hospitalized -- more than 100,000 Arizonans had tested positive for the virus and the state was facing an all-out surge.
What lead up to the summer surge?
The first coronavirus case in Arizona was detected in January, but no major mitigation efforts began in the state until March 2020.
On March 11, Gov. Doug Ducey signed an executive order announcing a state of emergency in Arizona.
The same day, Americans were shocked nationwide as the NBA announced it would suspend the remaining 2019-2020 season to prevent the spread of the virus.
Only nine cases had been identified in Arizona. Schools were closed, and students were told to go home and stay there.
By March 18, Banner Health, the state’s largest hospital system banned all visitors to area hospitals. Arizona, like many states was facing shortages in protective equipment for health care workers and individuals, so reducing the number of people in hospitals was a critical, though heartbreaking step.
By late March, the governor had ordered bars, gyms and movie theaters to close. Restaurants had permission to serve takeout or drive-thru services only. The governor ordered all “non-essential” workers to stay at home.
Many health care workers were distraught as hospitals and clinics had to halt elective surgeries. Thousands of health care workers faced furloughs.
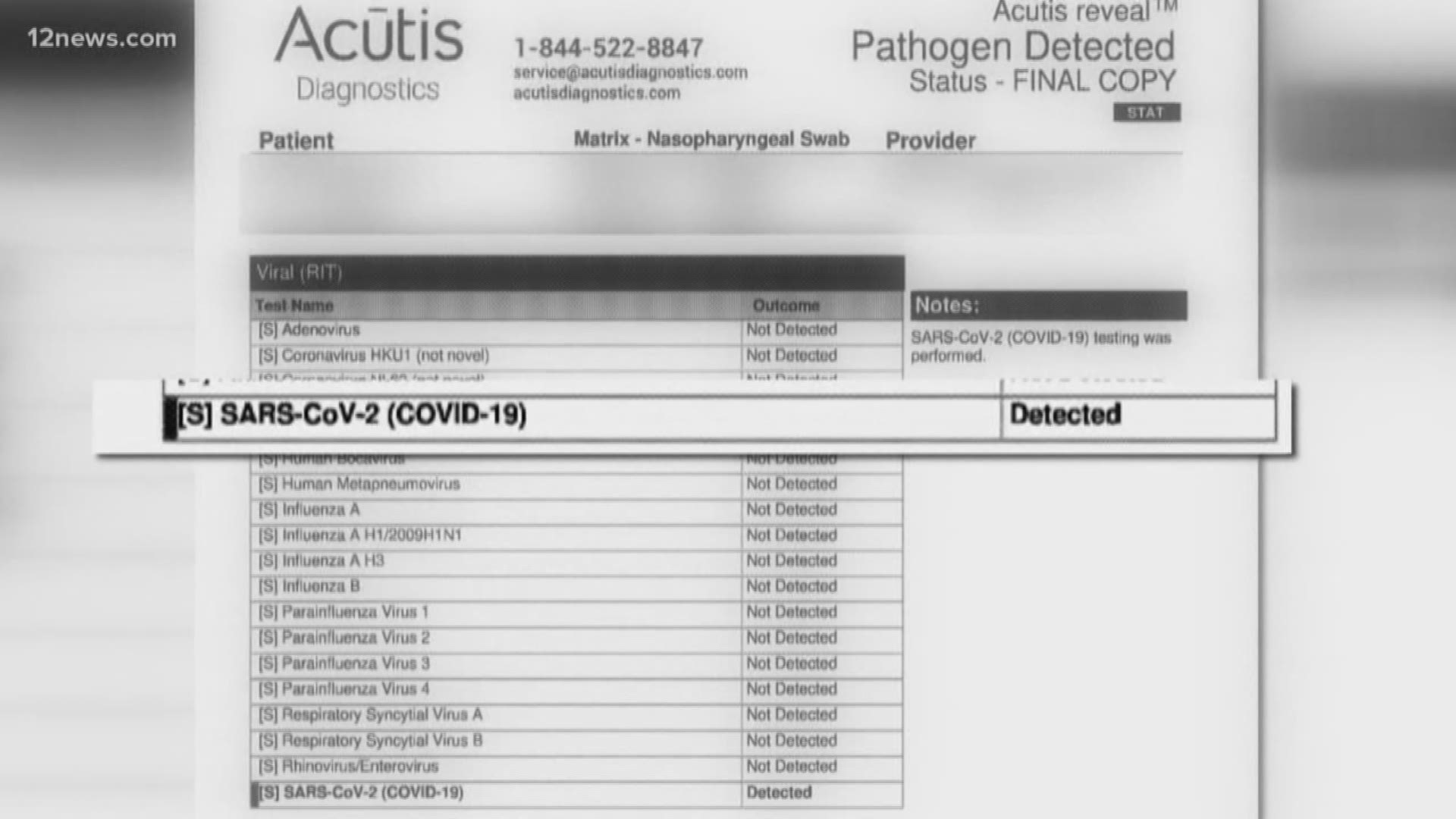
Still, cases continued to be detected, but slowly as many Arizonans reported extreme delays or errors in getting tested.
Arizona’s leaders agreed there weren’t enough tests to fully identify the spread of the virus, or to properly contact trace cases.
As of April 6, the state was prioritizing health care workers and first responders when allocating access to tests – even though the virus at this point was considered “widespread.”
Access to tests and timely results remained a problem for weeks, allowing the virus to spread through communities undetected.
On April 21, ADHS announced it had launched the Arizona Surge Line – a way for hospitals to communicate with one another and promptly move COVID-19 patients to a facility with more space or “appropriate level of care.”
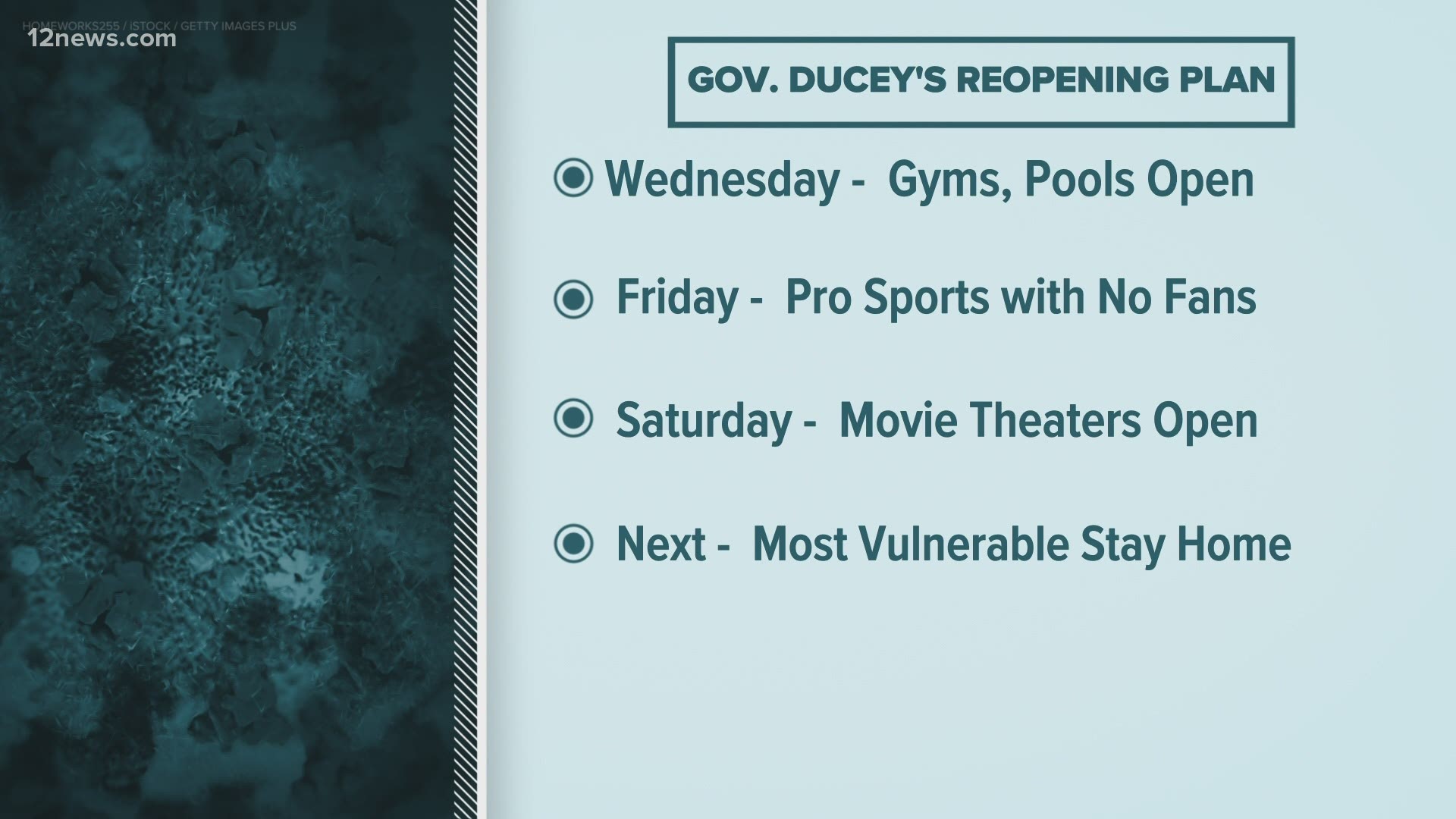
On May 15, Ducey allowed the state's stay at home order to expire, meaning salons, bars and gyms could reopen with social distancing measures. The enforcement of those rules, however, was left up to local governments.
The state had confirmed 13,169 positive cases of the virus and 651 Arizonans had already lost their lives.
In the following weeks, public health experts looked at the large crowds in recently-reopened bars as “super spreader” events – and warned that crowds celebrating the summer would likely lead to a surge in cases in June.
Those predictions proved correct.
System Overload
On June 1, the state passed 20,000 cases of coronavirus.
Ten days later, ADHS reported 10,000 more cases, totaling 31,264 in Arizona.
Ten days after that, on June 21, the ADHS reported 52,390 cases, 20,000 more in just 10 days’ time and 1,339 Arizonans had died.
On June 29, 2020, Gov. Doug Ducey and ADHS Director Dr. Cara Christ announced in a press conference that Arizona was activating the Crisis Standards of Care. These standards are a list of guidelines that help hospitals determine how to allocate limited resources.
And resources were limited.
Health department data showed COVID-19 patients accounted for 41% of all ICU beds across the state, and just 14% of ICU beds remained available statewide.
The governor also announced the state would again close bars, gyms and waterparks.
By the first of July, counties across the state began to enact mask mandates, though a statewide order was never issued.
Still, the number of hospitalizations and deaths would continue to climb.
Admitted To The Hospital
JULY 2: A first year of marriage, ending in disaster
William Curby called his new wife in late June saying he felt sick.
“I’m sick. I’m sweating, I’m freezing and I don’t feel good I need to go to urgent care. I told him I hope you don’t have COVID,” Trisha Curby, William’s wife, said.
The two had been married less than a year but had known each other for more than a decade.
“We met 14 years ago,” Trisha said. “The timing just wasn’t right. Here we are 14 years later and last year on June 1st (2019) we both started looking for each other on the same day.”
“At the spur of the moment, we got married.”
Their first year of marriage was filled with joy, but as their first anniversary approached William was admitted to Banner Boswell with COVID-19 on July 2. The new couple’s life together would change forever.
Days after he was admitted, Trisha worried William wasn’t receiving the care he needed. She had received a text message from him that stunned her.
“I’d rather just go home and die at peace with my wife and I’m like what is this about?” Trisha said. “The next call I got is my husband’s heart stopped and they forced him into a coma and onto a ventilator.”
JULY 8: Trouble breathing
Antonio Robles was admitted to Banner Thunderbird on July 8. He was struggling to breathe and had signs of COVID-pneumonia. He complained of a headache, which can be a common symptom of coronavirus.
He was given an IV-prescription drug, remdesivir, trade name Veklury. At the time, remdesivir was a promising but imperfect, experimental treatment for COVID-19 that the Food and Drug Administration allowed under an emergency use authorization for hospitalized COVID-19 patients.
The FDA would not approve Veklury until October 2020, and in July, the medication was in short supply.
Still, Antonio Robles began seeing his symptoms improve and was on a bi-pap machine, still able to communicate with his family, though they were not allowed to visit.
JULY 13: Testing delays, shortage in medication
Jason Betyou’s mother Helen was tested for COVID-19 on July 1, 2020. But she wouldn’t receive results back for 12 days, the same day she was admitted to the hospital.
It’s that delay, Jason fears, that may have contributed to his mother being denied access to the drug, remdesivir when she was hospitalized at Abrazo Arrowhead.
“I felt like my mom had the cards absolutely stacked against her,” Jason said. “That doctor says every COVID patient should get remdesivir and we have that via text but the administration said my mom couldn’t have it and that kills me.”
According to text messages Jason received from his mother’s healthcare provider, Abrazo Arrowhead’s hospital administration established guidelines that would only allocate remdesivir to those patients who had experienced symptoms for fewer than 10 days.
Abrazo Arrowhead did not answer 12 News’ questions about their policy regarding the allocation of remdesivir, but did say in a statement, “We are committed to providing every patient with excellent care in accordance with the patient’s treatment plan as determined by his or her physician and their clinical conditions. In the case of Covid, our physicians rely on recommendations made by the CDC, FDA and other expert bodies who have published official guidelines.”
“We won’t know what would’ve happened if she would’ve gotten it and that’s what’s kind of killing me inside,” Jason said.
Outside reinforcements
On July 17, Banner Health tweeted they were bringing in nearly 1,000 out of state nurses and respiratory therapists to assist in staffing shortages.
Still, Trisha worried William wasn’t receiving the care he needed. He had been on a ventilator since July 10, and so she was unable to speak with him or visit. His condition was worsening, she began searching for alternative options, to see if he could be transferred to another facility.
She turned to the Arizona Surge line where she said she learned a bed in another hospital was available.
“She was really nice and she told me they only had two beds left in Arizona for this ECMO or to get some type of experimental treatment. The process with Surge AZ was fairly simple,” Trisha said.
“I thought this is going to work, this is going to happen you know?”
Tony Robles began to worry about his father, Antonio, too.
By late July, he recorded phone calls with nurses and doctors he and his family spoke to after Antonio complained to his son that sometimes he would wait more than an hour for help after requesting someone come to his room.
“He’s all like ‘unfortunately I had an accident and they had to change me. They gave me new clothes.’ And I’m like you had an accident? What do you mean?” Tony recalled of a conversation with his father. “So I called them and I was very upset like hey how does this happen? He keeps telling me he presses the button but you guys are not going you know?”
In the recorded call, a nurse acknowledges Tony’s frustration, saying, “I know it’s hard for them to come right away just because again there’s just so many patients but they should be coming in a reasonable amount of time.”
Banner Health declined to comment on this story citing patient privacy laws.
In later calls, Tony and his family asked a healthcare worker directly, “is your staff overworked?”
The nurse responded: “Well I mean the answer is yes… because we're in a pandemic we don't have any beds we don’t have enough staff.”
In one exchange, the family received an even grimmer view:
“We have double the ICU beds for COVID than we ever had before so the two of the ICUs that we used to have, now we have double ICUs and most of it’s COVID. So these nurse are taking care of three and four patients but they have a nurse from another department assisting them.”
Antonio, who had been showing signs of improvement, took a serious turn for the worse. His medical records show that while he was beginning to overcome the virus, extensive sinusitis developed.
Instead of leaving the hospital, Antonio was placed on a ventilator. Tony Robles began searching for a transfer too.
For Jason, his mother Helen’s condition was causing similar concern. He began looking up alternative treatments for COVID-19 and asking what it might take to get his mother transferred.
“Nobody wanted to take her on and it killed me because you have this life saving treatment potentially however risky it is -- which as a family we communicated multiple times we were okay with the risk because we knew not taking the risk would lead to where we are today.” Jason said, in August. “No other doctor would take her.”
Tony, Trisha and Jason tried to have Antonio, William and Helen transferred. But none were able to find a higher standard of care.
Trisha said William’s doctor decided the alternative location she identified wasn’t a good fit.
“So my husband was not transferred and that bed was gone,” Trisha said.
“I called another hospital and they said unfortunately because he’s a COVID patient they couldn’t do that,” Tony said.
On July 25, Antonio Robles died from complications in the hospital.
Trisha Curby lost her husband William on July 27.
Helen Betyou continued fighting for another month, but lost her battle with coronavirus on August 26, 2020.
Each of these families hoped their experience could be a warning to the community when they first shared their stories.
RELATED: Arizona coronavirus cases dropped 75% after mask requirements put in place, CDC report shows
And cases did decline and level out in late summer. For several weeks from August through October, Arizona recorded fewer than 1,000 new cases per day.
But the lull didn’t last for long.
The Second Surge
By late October, new cases were again on the rise and hospital leaders were calling for more mitigation measures.
On Oct. 27, Banner Health released an email stating in part, “COVID-19 is spreading at its fastest rate since June,” continuing “We could meet or exceed the number of COVID-19 patients that we saw during Arizona’s surge in June and July.
Physicians, too, were raising red flags.
“Most of us feel like we’ve been screaming into the wind or tilting at windmills about this for months and months and months being unheard and when it is heard it’s usually too late,” said Dr. Brad Driefuss, an emergency room physician and co-founder of HCW Hosted, an organization created to support health care workers throughout the pandemic.
“Demoralizing is the word that comes to mind when you have an increase in patients and these are sick patients that take a lot of time, resuscitations that last hours,” Driefuss said. “It changes the standard of care. When you are only able to provide a level of care that is a fraction of what it was previously that contributes to the moral injury. The potential for medical errors go up significantly.”
On Oct. 28, Ducey held a press conference acknowledging a “storm was coming.” He would not hold another press conference for nearly three weeks until Nov. 18, when he stuck to a moderate approach to addressing the pandemic.
“Masks work, please wear them,” the governor said, as he further reiterated the mitigation measures that currently exist - including social distancing and capacity limitations in businesses and schools - and spoke of the public health guidance for having safe family gatherings during Thanksgiving.
“I am concerned about Thanksgiving. I anticipate we're seeing increased cases. We anticipate seeing a significant increase 10-14 days after Thanksgiving,” Dr. Cara Christ told 12 News in an interview in November.
Ahead of Thanksgiving, COVID-19 testing sites saw some of the highest numbers of people getting tested, presumably in an effort to have peace of mind before the holiday. However, small gatherings were likely a major contributor to the ongoing increases of cases and deaths through the month of December and early January 2021.
Yet a vaccine offered the first glimmer of hope in mid-December. Though there has been a slow rollout due to limited supply of the vaccine, as of Jan. 25, nearly 460,000 Arizonans received their first dose - and cases, once again, are showing signs of a slowdown.
In the year since the first case was identified, More than 725,000 Arizonans have tested positive for the coronavirus and more than 12,000 have lost their lives.
Their losses have changed their families, forever.
“I don’t want him to just be a number,” Trisha Curby said.
Call To Action
If you are seeking more information about how you can plan to keep you and your loved ones healthy and safe during the pandemic, some of the steps you already know.
Wear a mask.
Wash your hands.
Practice physical distancing - that is staying several feet away from others in public spaces.
For more specific planning options, HCW Hosted has created a “Health Citizens Pledge” that details steps you and your friends can take to establish a “social bubble” and make a “household plan” in case you or a member of your household does test positive for COVID-19.
The goal of the pledge is to reopen and restart responsibly, while saving lives and slowing the spread of COVID-19.
If you want to share your story with 12 News, contact us at connect@12news.com
All members of Team 12 have been committed to covering the coronavirus pandemic. Contributors to this report include Roberto Duarte, photojournalist and video editor, Carlos Chavez, photojournalist and Phillip Mathews, photojournalist.